Among the headlines for scant PPE, ventilators, and countless unknowns, the nature of transmission of the novel coronavirus, COVID-19, has posed additional risks for healthcare workers in the attempt to treat these patients. Thus far, respiratory viruses such as Sars-CoV 2 are not known to be transmitted via blood(1), and transmission via stool or vomitus is unknown(2). They are primarily transmitted via the respiratory tract and mucous membranes(2).
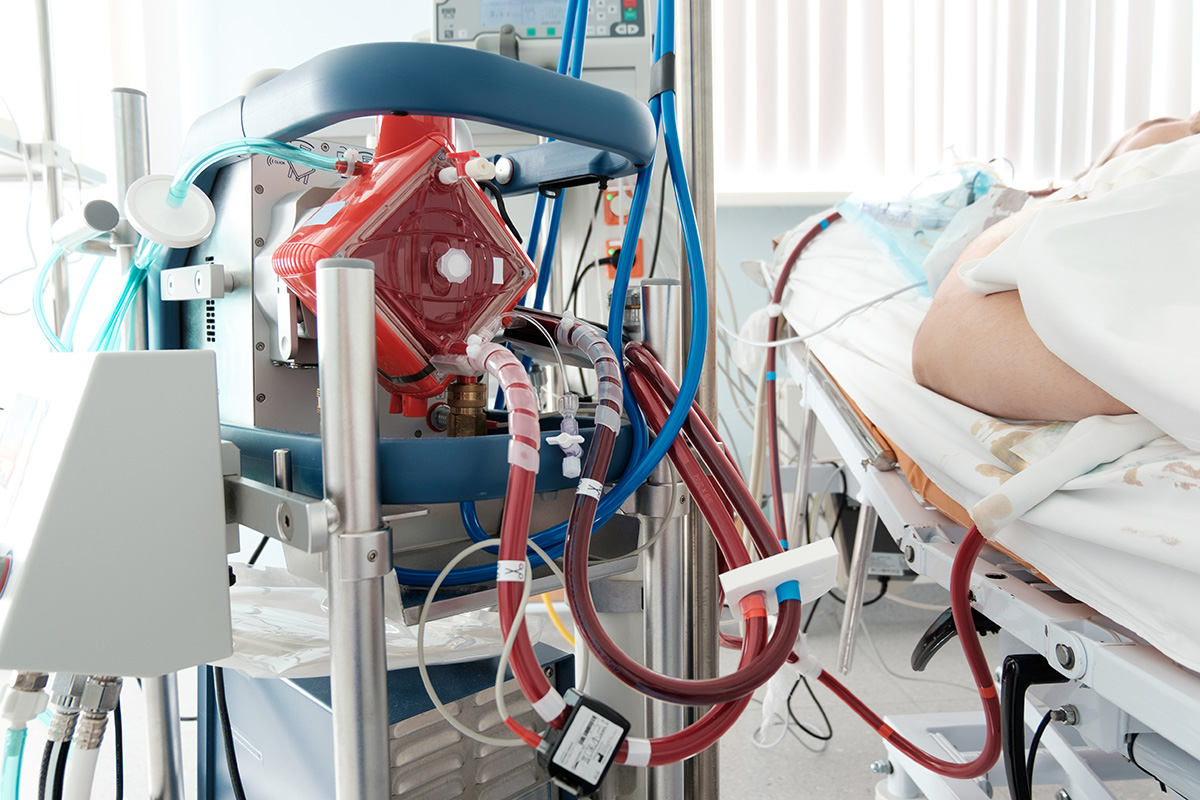
One feature term that many are now familiar with is ECMO. Extracorporeal membrane oxygenation (ECMO) is a treatment reserved for patients who did not respond to mechanical ventilatory strategies and other various options(3). This intervention includes running the patient’s blood through a circuit for oxygenation and returning it to the body. The device used for oxygenation contains hydrophobic hollow-fiber membranes, which “allow for the passage of gas through the fibers and into the blood while inhibiting the passage of plasma water into the gas phase” (4). These hollow fiber membranes are porous to plasma until the passage of plasma proteins, which eventually coat the micropores, causing direct blood to gas contact(4). According to the CDC and ELSO (the Extracorporeal Life Support Organization), there is no need to routinely collect the waste gases vented through the oxygenator; the term is appropriately named “scavenging.” Perfusionists typically use scavenging on cardiopulmonary bypass surgeries to protect themselves and the OR staff from waste anesthetic gases via the Boehringer VAVD controller.
In their official COVID Guidelines, ELSO states that ECMO patients should be cared for in a negative pressure room when possible. The only indication for the need to scavenge or additionally protect healthcare personnel is in the event of a plasma leak or damage to the oxygenators. For provided context, “most viruses range in size between 0.02 microns and 0.2 microns, and viruses in the Coronaviridae family (SARS, etc.) range in size between 0.08 and 0.15 microns” (4). While scavenging is not a requirement, should the quality of the oxygenator in question or negative pressure rooms be unavailable, it can easily be accomplished via the VAVD controller’s suction flowmeter.
Additional research can be found at the following resources:
- https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/coronavirus-disease-2019-covid-19-frequently-asked-questions
- https://www.elso.org/Portals/0/Files/pdf/ELSO%20covid%20guidelines%20final.pdf
- https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-extracorporeal-membrane-oxygenation-ecmo
- https://www.perfusion.com/scavenging-gas-outlet-ports-with-covid-19-ecmo-and-new-fda-recommendations-for-ecmo/
- https://www.fda.gov/media/136734/download
- https://www.covid19treatmentguidelines.nih.gov/introduction/
- https://www.elso.org/covid19
- https://ecmoedblog.files.wordpress.com/2020/04/schmidt_webina-ecmo-covid_elso.pdf
Back to Blog