Incontinence-associated dermatitis (IAD), sometimes referred to as perineal dermatitis, is an inflammation of the skin associated with exposure to urine or stool. IAD is one of four types of moisture-associated skin damage (MASD), defined as “inflammation and erosion of the skin caused by prolonged exposure to various sources of moisture, including urine or stool, perspiration, wound exudate, mucus, or saliva.”[1,2] It can range in severity from erythema with or without loss of skin integrity to infection. IAD effects are costly, painful, and, for the most part, preventable.
Healthy skin acts as a natural barrier against external harmful substances, pathogens, and moisture to prevent excessive liquid gain and loss from the body. The outermost part of the upper level of the skin, the stratum corneum, is the most crucial part of this barrier. The stratum corneum consists of corneocytes that are held together by desmosomes, creating a barrier that attracts and holds water and keeps a balance of skin bacteria and skin pH.
Suppose urine is in contact with the skin for prolonged periods. In that case, the moisture regulation becomes overwhelmed, thus disrupting the natural structure of the stratum corneum, which could result in maceration. Additionally, the urea in urine can break down skin bacteria, creating highly alkaline ammonia that shifts the skin’s pH. Fecal matter also contributes to an even more significant alkaline pH shift, thus causing damage to the stratum corneum. The introduction of pressure ulcers can quickly compound these issues, contributing to a deepening cycle of inflammation and skin breakdown. Additional complications may result if a secondary infection is introduced, fungal infection being the most common
IAD can be prevented and healed with timely and appropriate skin cleansing and skin protection. Prevention and treatment should focus on the proper use of incontinence containment materials. Although further research is required to evaluate the effectiveness of the various available interventions, it can be assumed that those solutions that result in a drier patient can effectively prevent IAD.
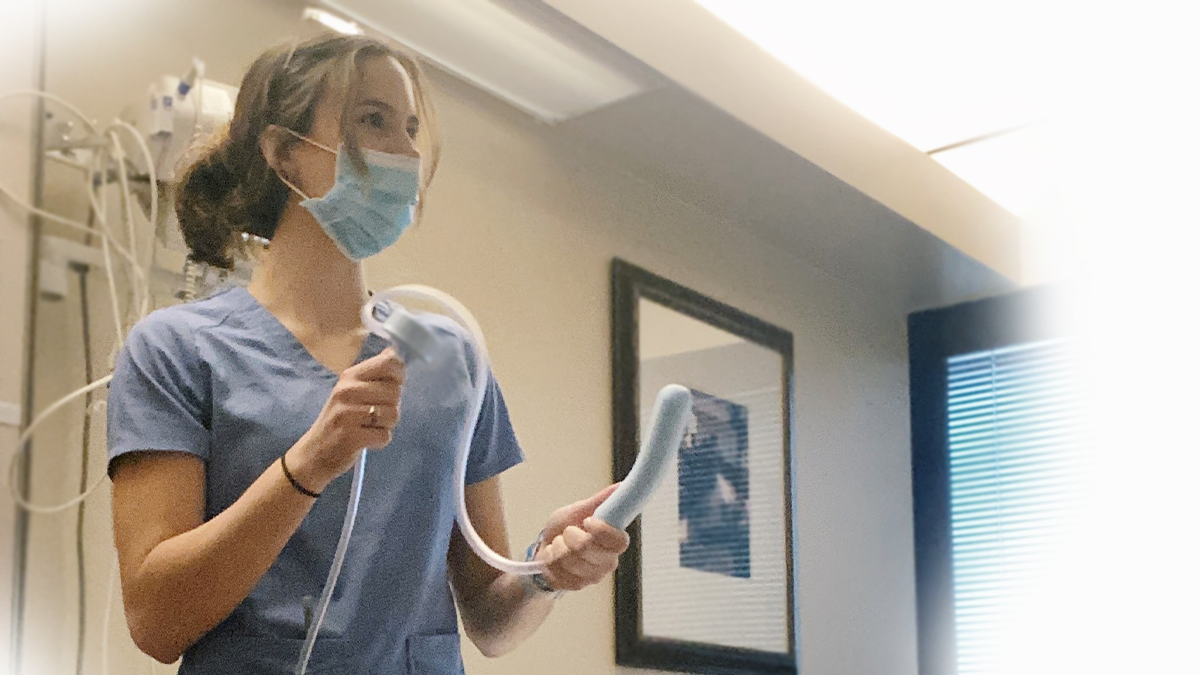
Looking for more information on intervention solutions? Be sure to check out the CareDry® System, non-invasive urinary management for women.
[1] Black JM, Gray M, Bliss DZ, et al. MASD part 2: incontinence-associated dermatitis and intertriginous dermatitis: a consensus. J Wound Ostomy Continence Nurs 2011;38(4):359-70.
[2] Gray M, Black JM, Baharestani MM, et al. Moisture-associated skin damage. Overview and pathophysiology. J Wound Ostomy Continence Nurs 2011;38(3):233-41.
“New insights on incontinence-associated dermatitis.” David Voegeli. 02 June 2017. https://www.independentnurse.co.uk/clinical-article/new-insights-on-incontinence-associated-dermatitis/155938/
Back to Blog